COURSE
SCIE1046: Fundamentals Of Microbiology With Lab
- About the Lab
Learning Objectives:
- Describe the structure of the Gram-positive and Gram-negative bacteria.
- Appreciate theoretical and technical aspects of the Gram staining procedure.
- Know the most commonly made mistakes in Gram staining.
- Critically interpret the results of a Gram staining experiment using a light microscope.
Estimated Length: 45 to 55 minutes
MAKE THE CONNECTION
The background information in section 2 was adapted from the following Microbiology lecture course Tutorials:
1.2.4 Preparing Slides for Microscopy
1.2.5 Staining Methods
2.1.2 Gram-Negative Bacteria
2.1.3 Gram-Positive Bacteria
5.5.7 Infections of the Nervous System
- Background Information
The following background information will be helpful as you prepare for the simulation.
In this lab, you will be using principles of Gram staining to identify a pathogen found in a cerebrospinal fluid (CSF) sample. A CSF sample is typically acquired using a lumbar puncture, often referred to as a spinal tap. A lumbar puncture is performed by inserting a needle between the L3 and L4 or L4 and L5 vertebra and extracting somewhere between 1 to 15 ml of CSF.
The brain and spinal cord are both covered in protective membrane layers. These layers are referred to as meninges (meninx singular). There are three layers of meninges. The top layer directly attaches to the bone of the cranium and the bone of the vertebral foramen and is known as the dura mater. Dura mater is Greek for “tough mother”. It is a very strong thick white tissue that protects the structures of the central nervous system (CNS). The middle layer is the arachnoid mater. Arachnid is a class of joint-legged invertebrate animals that include spiders. The arachnoid mater gets its name because this tissue is lined with spider-web-like vessels that nourish and care for the brain and spinal cord. The arachnoid mater forms a space above the underlying meninx, the pia mater. This space is referred to as the subarachnoid space. CSF flows freely in this space, providing a protective cushion to CNS structures. The deepest meninx layer, the pia mater adheres directly to CNS structures and is very thin. Pia mater is Greek for “gentle mother” and is semi-permeable, allowing only select molecules to cross the membrane into the CNS tissues.
CSF flows through the subarachnoid space and drains through the ventricles in the brain. These ventricles are open spaces that allow for continuous circulation of CSF. As CSF flows in the subarachnoid space, it not only creates a protective cushion, it also picks up waste from the tissues.
The blood–brain barrier is a collection of cells that serve as a barrier between nervous system vessels and the CSF. Only pathogens with specific characteristics can cross the blood–brain barrier and reach the CSF. Pathogens can reach the CSF through four main methods: transcellular, paracellular, phagocyte piggyback, or non-hematogenous. You can learn more about these methods by reading section 5.5.7 in the microbiology lecture course.
2a. Gram Staining
The Gram stain procedure is a common and important type of differential staining. It classifies bacteria into one or two groups based on characteristics of their cell walls. This procedure was developed by Danish microbiologist Hans Christian Gram in 1884.
STEP BY STEP
- The first stain applied is called the primary stain. Crystal violet is added. This stains all of the cells purple.
- Next, Gram’s iodine is added as a mordant(a substance used to set or stabilize stains or dyes). Gram’s iodine complexes with the crystal violet to form a crystal violet–iodine clump that is harder to remove from thick layers of peptidoglycan (a carbohydrate) in cell walls.
- Next, the slide is rinsed with a decolorizing agentthat helps wash out the stain. Ethanol or an acetone/ethanol solution is most commonly used. Cells with thick peptidoglycan layers retain the original crystal violet stain much more easily during this step than cells with thin peptidoglycan layers.
- Finally, a secondary counterstain(a stain added after another stain to contrast with it in some way) is added. Safranin is most commonly used, and it stains the decolorized cells pink. The cells that have retained the crystal violet dye are affected much less noticeably.
Cells that retain crystal violet and remain purple are called gram-positive, and cells that lose crystal violet and become pink when dyed with safranin are called gram-negative. These differences reflect the differences in the peptidoglycan layer, but there are other important differences between gram-positive and gram-negative cells. You will learn more about these in the lessons about prokaryotic cells and the characteristics of taxonomic groups of bacteria.
IN CONTEXT
There are several considerations to remember when using the Gram staining procedure. First, it is important to use young, healthy colonies because older bacterial cells may have damaged cell walls that do not retain the primary stain as well as healthy cells do. Second, errors such as leaving the decolorizer on too long can affect the result. In some cases, most cells will appear gram-positive, while a few will to be gram-negative. This suggests damage to the individual cells or that the decolorizer was left on too long. The cells should still be classified as gram-positive if they are all the same species.
Besides their differing interactions with dyes and decolorizing agents, the chemical differences between gram-positive and gram-negative cells have implications with clinical relevance. Therefore, Gram staining is a valuable clinical tool, and knowing how to use it is an important skill.
EXAMPLE
Gram staining can help clinicians classify bacterial pathogens in a sample into categories associated with specific properties. This can be helpful in selecting an appropriate antibiotic. You will learn more about the characteristics of gram-positive and gram-negative bacteria and about antibiotics in other lessons.
REFLECT
Most people have taken antibiotics at some point. Can you remember some of the antibiotics that you have been given? What do you think the doctor considered when deciding which antibiotics to use? Think about this, and pay attention the next time you or someone you know is given antibiotics.
| Gram Staining Process | ||||
| Gram Staining Steps | Cell Effects | Gram-Positive | Gram-Negative | |
| Step 1 Crystal violet The primary stain is added to the specimen smear. |
The cells are stained purple or blue. | |||
| Step 2 Iodine The mordant makes the dye less soluble, so it adheres to cell walls. |
The cells remain purple or blue. | |||
| Step 3 Alcohol/Acetone The decolorizer washes away the stain from gram-negative cell walls. |
Gram-positive cells remain purple or blue. Gram-negative cells are colorless. |
|||
| Step 4 Safranin The counterstain allows dye adherence to gram-negative cells. |
Gram-positive cells remain purple or blue. Gram-negative cells appear pink or red. |
|||
In the specimen shown in the image below, the gram-positive bacterium Staphylococcus aureus retains the crystal violet dye even after the decolorizing agent is added. Gram-negative Escherichia coli, the most common Gram stain quality-control bacterium, is decolorized and is only visible after the addition of the pink counterstain safranin.
Source: modification of work by Nina Parker.
EXAMPLE
Gram staining is often used as a first step in identifying bacteria in the lab. Knowing whether a bacterial infection is gram-positive or gram-negative can be helpful in choosing an effective antibiotic.
The micrograph shows Pseudomonas aeruginosa. Is this species gram-positive or gram-negative? Because the rods are light pink, the color of the safranin counterstain, this micrograph shows that P. aeruginosa is gram-negative.
TRY IT
After the Gram staining technique is used on a sample of bacteria, the cells appear light pink. However, the bacterial species is known to be gram-positive.
What is a possible explanation for this finding?
TERMS TO KNOW
Primary Stain
The first stain added in a series of stains.
Mordant
A substance used to set or stabilize stains or dyes.
Decolorizing Agent
A chemical that helps wash out a stain.
Counterstain
A stain added after another stain to contrast with it in some way.
2b. Preparing Slides for Microscopy
You are encouraged to review the complete Microbiology lecture course Tutorial 1.2.4 Preparing Slides for Microscopy for background on this topic before you begin the simulation.
2c. Gram-Negative Bacteria
You are encouraged to review the complete Microbiology lecture course Tutorial 2.1.2 Gram-Negative Bacteria for background on this topic before you begin the simulation.
2d. Gram-Positive Bacteria
You are encouraged to review the complete Microbiology lecture course Tutorial 2.1.3 Gram-Positive Bacteria for background on this topic before you begin the simulation.
- Lab Manual
Lab Manual – The Gram Stain: Identify and differentiate bacteria
This Lab Manual gives a synopsis of the lab and the theory behind it. You’re encouraged to read or download the manual before launching the lab. This information will also be available during the simulation by selecting the “Theory” tab on the virtual LabPad.
4. Launch Lab
You’re ready to begin! Review the helpful navigation tips below. Then click the Launch Lab button to start your lab. Be sure to answer all the questions in the simulation because they contribute to your score. Good luck, scientists!
- Exiting: To exit a lab simulation, press the ESC key on your keyboard. This key returns you to the objective screen for the simulation.
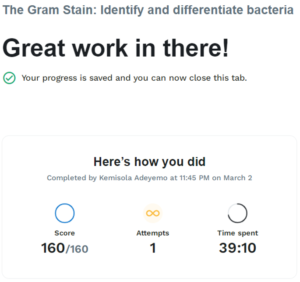
- Saving: You do not need to complete a simulation in one sitting. Labster saves your progress at predetermined checkpoints upon exit. To see your progress at any time, click on the mission tab of the LabPad.
- Restarting: You are allowed an unlimited number of restarts for a simulation to improve your quiz score. Sophia and Labster will always store your best score.
- Just Browsing: You can restart a simulation to have a look around without completing it. The program will still retain your previous (and best) score.
